Complete Story
04/12/2024
Priority Health Update
Priority Health Managed Care Committee Member
Flora Werle - Cancer & Hematology Centers of West Michigan
Click here to visit the Priority Health Provider News Page for additional updates.
Appeals on incorrectly coded claims will result in upheld denials starting May 1
Accurately coding claims the first time helps to ensure timely claim processing and reimbursement and avoids the need for appeals. In support of this and in alignment with industry standards, we’re making the following update to our claim appeals process.
Effective May 1, 2024, appeals received on incorrectly coded claims will result in the denial being upheld. Remember, you only have one opportunity to appeal per claim.
If your claim isn’t correctly coded when you first submit it, submit a corrected claim with the accurate coding.
Things to keep in mind
Accurately coded claims often need the following (note this isn’t an exhaustive list):
- Coding the diagnosis to the highest level of specificity
- Using the correct place of service (POS) code
- Appending the appropriate, required modifiers for services rendered
Healthy Living and Solara network termination
Two of our diabetic supply providers are being removed from our network: Healthy Living Medical Supply and Solara Medical Supplies. To ensure our members—your patients—continue to receive the diabetic supplies and equipment they need, please begin referring patients to other diabetic supply providers in the Priority Health network and transfer all current prescriptions to in-network suppliers.
When is this change taking effect?
Healthy Living and Solara will no longer be in our network effective August 15, 2024. However, authorizations for supplies with these companies will no longer be approved after April 30, 2024.
Which members will be impacted?
This change impacts commercial and individual, Medicare and Medicaid members who use these two companies.
Why are we making this change?
We’re removing these two suppliers from our network because they are not able to meet the standards we’ve set for serving our members.
What do you need to do?
Please begin transitioning your patients’ diabetic supply prescriptions to one of the in-network providers listed below. After April 30, you’ll only be able to refer our members to these companies. If the member already has a prescription with Healthy Living or Solara, along with a valid authorization, the prescription will be honored until August 15.
- CareLinc
888.810.5462
carelincmed.com - J&B Medical
800.737.0045
jandbmedical.com - Byram Healthcare
877.902.9726
byramhealthcare.com - Medtronic (Medtronic CGM, pump and supplies only)
800.633.8766
medtronicdiabetes.com - Tandem (Tandem pump and supplies only)
877.801.6901
tandemdiabetes.com - Real-Time Medical Supply
248.537.2922
realtimemedicalsupply.com
What about CGMs?
For fully funded commercial (group and individual) members, Dexcom and Freestyle Libre continuous glucose monitors (CGMs) and related supplies can only be obtained through the pharmacy benefit, effective upon their 2024 plan renewal date. The network change communicated in this letter doesn’t impact that previously communicated CGM benefit change.
Get our 2024 HEDIS® ECDS Provider Guide
Our new Healthcare Effectiveness and Data Information Set (HEDIS®) Electronic Digital Data Source (ECDS) Provider Guide is now available. This guide will help you better understand HEDIS ECDS reporting and its impact on your patients, your practice and our health plan.
Why is ECDS important?
The National Committee for Quality Assurance (NCQA) implemented ECDS to help move measures toward a more digital future. ECDS reporting is part of NCQA’s larger strategy to enable a digital quality system and is aligned with the industry’s move to digital measures.
What’s included:
Each HEDIS ECDS measure includes:
- A description of the measure
- Correct billing codes for claims submissions
- Tips and best practices to help close care opportunities and improve your HEDIS rate
To access the guide, log into your prism account and navigate to Provider Incentive Programs, then Quality Improvement.
Safely dispose of unneeded prescription drugs on April 27
Saturday, April 27, is National Prescription Drug Take Back Day and we’re proud to join thousands of sites across the country once again as a take back site. We welcome your patients and all members of our community to stop by between 10 a.m. – 2 p.m. to drop off their expired, unwanted or unneeded prescription medications for safe disposal.
Priority Health
3111 Leonard St NE
Grand Rapids, MI 49525
At last year’s April event, we collected 584 pounds of medication and distributed 126 NARCAN® kits at our sites.NARCAN kits will be distributed again this year.
Why hold Take Back events?
Take Back programs offer a safe way to dispose of unused prescription drugs. Unused or expired prescription medications are a public safety issue and can lead to accidental poisoning, overdose and potential misuse.
Download our Takeback Day flyer
Have patients affected by substance use conditions?
Our behavioral health department has clinical staff who specialize in helping members manage complex and chronic mental health and substance use conditions. Our care coordination team is available to support your patients while you help them access inpatient or outpatient treatment.
Encourage your patients to use Teladoc Health Mental Health
Teladoc Health is a digital tool that offers over 1,400 self-directed activities on a variety of mental wellness topics including alcohol and drug recovery as well as opioid recovery. These tools are available to our members 24/7 and complement the care you provide them. Encourage your patients to sign up for a free account today.
New provider-based billing reimbursement policy goes into effect June 1
In alignment with industry standards, we’re updating our provider-based billing reimbursement practices.
What’s changing?
Effective June 1, we’ll no longer separately reimburse for clinic fees or any other fees associated with space used to provide E/M services, when billed on a UB-04 facility claim, regardless of the office being located on the hospital campus and/or using the hospital TIN.
This update will apply to all commercial and Medicaid lines of business for in- and out-of-network providers and facilities (excluding RHC and FQHC), regardless of reimbursement methodology.
What do you need to know?
We’ve published a new provider-based billing policy to support you in understanding:
- What’s included in both non-facility and facility reimbursement rates
- How these rates apply to a claim based on the place of service (POS) code
- The conditions under which a claim will be denied
You should continue to bill the most appropriate place of service (POS) code for services rendered in your practice setting.
April 2 Change Healthcare outage update
Submitting claims
We're seeing closer to normal claims volumes as providers have switched to new clearinghouses or submitted paper claims. We don’t recommend holding claims. You can switch to a new clearinghouse or submit on paper.
We’ve recently added Optum iEDI and Availity clearinghouses, and we also work with multiple other clearinghouses, like Waystar, if you choose to switch.
Remittance advices (RAs)
RAs are being sent through Optum again but not yet through Change Healthcare. You can also get RAs through Filemart if you already have Filemart set up and use this to get RAs.
Authorizations
There’s no impact to authorizations. Continue submitting authorizations as usual.
Paper checks
Paper checks for claims payment as well as capitation and admin payments have begun mailing. Please keep your check stubs so you’re able to match the check reference ID number to RAs when they arrive. We’re working quickly to get RAs for paper check claims payments mailed to you separately.
As always, you can sign up for electronic funds transfer to start the process for electronic payments.
Change Healthcare outage communications archive
Visit our news & education page for an archive of communications we've sent about the Change Healthcare outage.
We’re reprocessing certain ABA service claims submitted from Jan. 1 to March 1, 2024
We’re reprocessing claims for Applied Behavior Analysis (ABA) services for CPT code 97153 submitted for commercial and individual members from Jan. 1 through Mar. 1, 2024. These claims originally paid at the 2023 rate and are being reprocessed to pay providers at the increased 2024 rate.
There’s no need to resubmit claims.
Impacted claims submitted as of Mar. 2, 2024, are being reprocessed at the higher 2024 rate automatically. Refer to our provider manual to learn about our timeline and process for correcting payments.
Did you know?
ABA rate increases and a newly covered code Below is an overview of our ABA code reimbursement rates for commercial plans, several of which were increased this year to support our provider network.
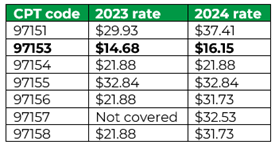
Additionally, as of Jan. 1, 2024, we began covering CPT code 97157 for all group commercial plans, allowing providers to offer training and support in a group setting with parents and caregivers whose family members are receiving ABA services.
See our Autism Spectrum Disorders medical policy for more information.
Change Healthcare update: Paper claims checks mail week of March 25, new clearinghouse set up, ERAs on
Paper claims started mailing week of March 25
Paper checks for claims payments, which were delayed due to the Change Healthcare outage, started processing the week of March 25. We expect it to take multiple weeks to process all pending payments.
These checks will look different than other checks, and the check number will not match the information on the RA when we're able to send those.
Keep your check stubs. Remittance advices (RAs) are not yet available. We’ll mail these separately as soon as possible. Your check stub, which will have a check reference ID number, will help you match your checks to the RAs.
As always, you can sign up for electronic funds transfer to start the process for electronic payments. Electronic payments were not impacted by the Change Healthcare outage.
New clearinghouse—Optum iEDI—now available to send claims
We have a new clearinghouse available. Optum iEDI is now directly connected to Priority Health and sending us claims.
We work with multiple clearinghouses if you choose to switch to get claims sent to us.
Electronic RAs restarting through Optum; still not sending through Change Healthcare
If you received electronic remittance advices (RAs) through Optum, you’ll start receiving these again. Note that Optum and Change Healthcare are separate clearinghouses. Only the Optum channel is restarting now.
You can get RAs through Filemart if you already have a Filemart set up and use this to get RAs. You can also switch to a new clearinghouse. If you choose to switch to a new clearinghouse, please visit our provider page for more information on updating or submitting the request for electronic remittance advice (ERA) setup.
See our latest news items about the Change Healthcare outage:
- Feb. 22: prism and pharmacy claims impacted by Change Healthcare major incident
- Feb. 26: Ongoing impacts from the Change Healthcare outage
- Feb. 28: Other clearinghouses available
- March 4: Clarification on clearinghouses
- March 18: Availity clearinghouse now set up, cap and admin payments releasing this week
Report Broken Links
Have you encountered a problem with a URL (link) on this page not working or displaying an error message? Help us fix it!
